THE School Deserts Index:
How Education Shortages Are Stifling America’s Clinical Workforce
Download PDF VersionAbstract/Brief:
A Growing Allied Health Workforce Shortage—Fueled by Diminishing Training Access
Across the U.S., hospitals are grappling with critical staffing shortages in allied health roles—positions that are essential for both patient care and hospital revenue generation. The root cause? A severe lack of local training programs. It’s not just that demand for these roles is growing faster than supply. In many parts of the country, the infrastructure to train new talent is disappearing. Fewer schools mean fewer graduates, making it harder to hire locally or build a stable, long-term workforce.
At Clasp, we partner with healthcare systems to widen their allied health talent pipelines by connecting them with qualified students before they graduate and incentivizing 3+ years of retention. Through this work, we’ve identified a troubling trend: School Deserts—regions where the demand for healthcare professionals exceeds the number of new talent entering the workforce, due to limited or no access to local education and training pathways. To better understand the scope of the problem, we developed the School Deserts Index Report, a first-of-its-kind, state-by-state analysis that highlights where these deserts exist, their economic impact, and what healthcare leaders can do to protect the long-term health of their workforce.
With nearly 99 million Americans living in Health Professional Shortage Areas (HPSAs), and demand for clinical professionals expected to outpace supply by over 100,000 by 2028, the need for action is urgent. School deserts are quietly exacerbating workforce shortages by cutting off local talent pipelines, driving up vacancy rates, and increasing reliance on costly contract labor.
🔎 What’s Inside This Report
- Key demographic trends driving school deserts
- Which states are hardest hit by training access gaps—and what the fallout looks like
- Role-by-role analysis of where shortages are growing fastest and why
- New data on school program concentrations and their mismatch with care delivery needs
- The true cost of school deserts to healthcare employers
- Tactical playbook for health system leaders—including actionable strategies for rural workforce growth
🚨 Key Findings
- Some states (e.g., Wyoming, Alaska, Maine) have zero in-state programs for vital roles like physical therapists or surgical technologists.
- Nearly 30% of U.S. counties lack a single allied health training program.
- Even where programs exist, distance, housing, and clinical capacity make enrollment impossible for many rural learners.
- School deserts directly correlate with increased turnover, reliance on travelers, and delays in care delivery—especially in ORs and ICUs.
🏥 Real Systems, Real Strain
- In Colorado, rural hospitals in San Luis Valley report 2–3 hour commutes for students, limiting placements and creating chronic shortages.
- Florida expects to face a deficit of 1,616 surgical technologists and 2,630 physical therapists by 2030.
- In New Mexico, a projected 52% shortfall in allied health workers by 2035 is already being felt in tribal and frontier regions.
🚀 What Happens Next
Allied health roles make up nearly 60% of the U.S. healthcare workforce—but the infrastructure to train them is dangerously uneven. If hospital leaders don’t act now, clinical deserts will grow—and care delivery will suffer.
Clasp’s School Deserts Index report is a call to action for health systems, payers, and policymakers: Build locally. Fund smarter. Retain longer.
📬 Want to dig into your state’s risk profile—or build and retain your own allied health pipeline? Reach out to us at marketing@clasp.com or download the full report now.
School Deserts Index
This table reflects Clasp’s School Desert Impact Index, focused specifically on student pipeline risk rather than current workforce counts. The Workforce Coverage Gap metric compares expected graduates to projected demand — signaling states where incoming talent alone is unlikely to keep pace. In other words, it highlights future shortages at risk of emerging as the current workforce turns over, rather than today’s total workforce gap (which is what the maps address). The color shading provides a quick visual of which roles and states face the steepest student‑supply shortfalls.
Note: Some states might look like they have a more stable healthcare workforce because their overall demand is lower—even if they still have shortages. On the other hand, bigger states with large cities and lots of training programs might actually have bigger workforce gaps when you look at the percentage of demand they can’t meet.
Key: 🔴Critical, 🟠High, 🟡Moderate, 🟢Low
| Impact Index | State | PT | Surg Tech | Rad Tech | RT | Lab Tech | CRNA | Workforce Coverage Gap (%) |
|---|---|---|---|---|---|---|---|---|
| 1 | Oregon | 🟠 | 🔴 | 🔴 | 🔴 | 🔴 | 🔴 | 49% |
| 2 | Alaska | 🔴 | 🔴 | 🔴 | 🔴 | 🟠 | 🔴 | 37% |
| 3 | New Jersey | 🔴 | 🔴 | 🔴 | 🔴 | 🟠 | 🔴 | 29% |
| 4 | Washington | 🔴 | 🔴 | 🔴 | 🔴 | 🟠 | 🔴 | 42% |
| 5 | Delaware | 🟡 | 🔴 | 🔴 | 🔴 | 🔴 | 🔴 | 44% |
| 6 | Vermont | 🟠 | 🔴 | 🟠 | 🔴 | 🔴 | 🔴 | 38% |
| 7 | New York | 🟠 | 🔴 | 🔴 | 🔴 | 🟠 | 🔴 | 32% |
| 8 | Maryland | 🔴 | 🔴 | 🔴 | 🔴 | 🟡 | 🔴 | 35% |
| 9 | New Hampshire | 🟡 | 🔴 | 🟠 | 🔴 | 🔴 | 🔴 | 41% |
| 10 | Virginia | 🟠 | 🔴 | 🔴 | 🔴 | 🟡 | 🔴 | 26% |
| 11 | Nevada | 🟠 | 🔴 | 🔴 | 🟡 | 🔴 | 🔴 | 44% |
| 12 | Rhode Island | 🟠 | 🔴 | 🔴 | 🔴 | 🟡 | 🔴 | 28% |
| 13 | Hawaii | 🟢 | 🔴 | 🔴 | 🔴 | 🟠 | 🔴 | 47% |
| 14 | Illinois | 🟠 | 🟠 | 🟠 | 🔴 | 🟠 | 🔴 | 25% |
| 15 | Wyoming | 🔴 | 🟡 | 🟠 | 🔴 | 🟠 | 🔴 | 26% |
| 16 | New Mexico | 🔴 | 🟠 | 🟠 | 🟠 | 🟠 | 🔴 | 34% |
| 17 | Colorado | 🔴 | 🟡 | 🔴 | 🟠 | 🟠 | 🔴 | 23% |
| 18 | Connecticut | 🟠 | 🔴 | 🔴 | 🔴 | 🟡 | 🟠 | 23% |
| 19 | Massachusetts | 🟡 | 🔴 | 🔴 | 🔴 | 🟢 | 🔴 | 9% |
| 20 | California | 🟠 | 🟠 | 🔴 | 🟡 | 🟠 | 🔴 | 34% |
| 21 | Pennsylvania | 🟡 | 🔴 | 🔴 | 🔴 | 🟠 | 🟡 | 26% |
| 22 | Arizona | 🟠 | 🟠 | 🟢 | 🔴 | 🟠 | 🔴 | 28% |
| 23 | Montana | 🟡 | 🟡 | 🟠 | 🔴 | 🟠 | 🔴 | 22% |
| 24 | Iowa | 🟠 | 🟠 | 🟡 | 🔴 | 🟡 | 🔴 | 15% |
| 25 | Georgia | 🟠 | 🟡 | 🟠 | 🟠 | 🟠 | 🔴 | 27% |
| 26 | Maine | 🟡 | 🔴 | 🟠 | 🔴 | 🔴 | 🟢 | 33% |
| 27 | South Carolina | 🟠 | 🟡 | 🔴 | 🔴 | 🟠 | 🟡 | 35% |
| 28 | Indiana | 🟠 | 🟠 | 🟡 | 🟠 | 🟡 | 🔴 | 18% |
| 29 | Wisconsin | 🟡 | 🟡 | 🔴 | 🔴 | 🟡 | 🟠 | 16% |
| 30 | Ohio | 🟠 | 🟠 | 🟠 | 🟠 | 🟡 | 🟠 | 17% |
| 31 | Michigan | 🟠 | 🟡 | 🔴 | 🔴 | 🟠 | 🟢 | 31% |
| 32 | Oklahoma | 🟠 | 🟢 | 🟠 | 🟠 | 🟡 | 🔴 | 25% |
| 33 | Mississippi* | 🔴 | 🟢 | 🟡 | 🟠 | 🟡 | 🔴 | 0% |
| 34 | Missouri | 🟡 | 🔴 | 🟠 | 🔴 | 🟢 | 🟡 | 17% |
| 35 | North Carolina | 🟠 | 🟠 | 🟠 | 🔴 | 🟡 | 🟢 | 25% |
| 36 | Minnesota | 🟠 | 🟠 | 🟠 | 🔴 | 🟡 | 🟢 | 17% |
| 37 | Louisiana | 🔴 | 🟡 | 🟡 | 🔴 | 🟠 | 🟢 | 25% |
| 38 | Texas | 🟠 | 🟡 | 🟡 | 🟠 | 🟡 | 🟠 | 19% |
| 39 | Utah* | 🟠 | 🟡 | 🟠 | 🟡 | 🟢 | 🔴 | 0% |
| 40 | Florida | 🟠 | 🟡 | 🟠 | 🔴 | 🟡 | 🟢 | 25% |
| 41 | Tennessee | 🟡 | 🟠 | 🔴 | 🔴 | 🟢 | 🟢 | 16% |
| 42 | D.C. | 🟢 | 🔴 | 🔴 | 🟠 | 🟢 | 🟢 | 15% |
| 43 | Alabama | 🟠 | 🟡 | 🟠 | 🔴 | 🟢 | 🟢 | 19% |
| 44 | Nebraska | 🟢 | 🟡 | 🟠 | 🟠 | 🟠 | 🟢 | 5% |
| 45 | Idaho* | 🔴 | 🟢 | 🟢 | 🟢 | 🟡 | 🔴 | 0% |
| 46 | Kansas | 🟠 | 🟢 | 🟠 | 🟡 | 🟢 | 🟠 | 2% |
| 47 | South Dakota* | 🟠 | 🟢 | 🟡 | 🔴 | 🟢 | 🟢 | 0% |
| 48 | Kentucky | 🟠 | 🟢 | 🟠 | 🟡 | 🟢 | 🟡 | 1% |
| 49 | West Virginia | 🟠 | 🟢 | 🟠 | 🟡 | 🟡 | 🟢 | 9% |
| 50 | Arkansas | 🟡 | 🟢 | 🟢 | 🟢 | 🟠 | 🟠 | 4% |
| 51 | North Dakota* | 🟢 | 🔴 | 🟢 | 🟡 | 🟢 | 🟢 | 0% |
*States with role-specific shortages but no overall workforce shortfall. These states have a net neutral healthcare workforce, though certain roles may still face localized shortages.
Introduction
Allied health professionals keep our healthcare system running—handling everything from diagnostics to patient recovery. But across the country, especially in rural and underserved areas, we're seeing growing shortages in these essential roles.1 Take Certified Registered Nurse Anesthetists (CRNAs), for example, they play a vital role in delivering anesthesia care before, during, and after procedures. Yet by 2033, the U.S. is expected to fall short by around 12,500 anesthesia providers.² For for reference, the US currently only graduates approximately 2,400 nurse anesthetists per year and given the limited school infrastructure, <25% of applicants for CRNA programs are accepted.
One of the root causes of these shortages? School deserts: regions where students have no realistic access to accredited training programs.
Without nearby schools, students are less likely to pursue clinical careers in respiratory therapy, surgical technology, physical therapy, and other essential fields. Communities, in turn, lose out on local talent—leading to higher vacancy rates, deeper reliance on travel staff, and weakened continuity of care.
This report identifies where these school deserts are most severe and offers actionable solutions for hospital executives, workforce planners, and policymakers who want to stabilize their pipelines and strengthen care delivery in high-need areas.
Ashley, a new mom in West Michigan, was in excruciating pain as she tried to adjust to motherhood. After finally getting an ultrasound appointment she learned she would need to anxiously wait more than 80 days before her images would be reviewed and she would get any answers. Across the country stories like Ashley’s are becoming more common as school deserts leave pockets of the country without the clinicians they need.
What Are School Deserts?
School deserts are geographic areas lacking accessible, accredited allied health training programs. They disproportionately affect rural and underserved regions—where hospitals are already stretched thin—and limit the ability of students to train close to home.
Common barriers include:
- No local training or clinical placement options
- Long travel distances for in-person programs
- Weak broadband access for hybrid learning
- Housing or transportation challenges for students
Without proximity, students don’t enroll—and if they leave to train elsewhere, they often don’t return. These bottlenecks are a leading driver of chronic staffing shortages in roles like:
- Respiratory Therapists
- Radiologic Technologists
- Surgical Technologists
- Physical Therapists
- Medical Laboratory Technicians
- Nurse Anesthetists
What’s Driving the Rise of School Deserts?
There’s no single reason school deserts exist—but a few key trends are making them worse, especially in rural and underserved areas.
- Demographic Shifts and Workforce Gaps: Across the U.S., the healthcare workforce is aging faster than it’s being replaced. The average U.S. physician is over 50, and many allied health professions are seeing similar trends.4 At the same time, younger populations—especially those aged 20–34 are unevenly distributed.5 Some rural regions are losing young people to larger metro centers, while many cities face high demand for programs but lack the capacity to train enough students.
- Education Access Mismatches: Many communities simply don’t have nearby allied health training programs. In urban areas, capacity constraints, cost of living, and long waitlists can be barriers. In suburban and rural regions, programs may not exist at all or may be located too far away to be practical. These gaps in program availability leave entire counties and metro zones without sufficient options for local talent to enter the field.6
- Infrastructure and Connectivity Barriers: Online and hybrid education options could help fill the gap—but not everyone can access them. While rural communities often face broadband connectivity issues, urban students may struggle with device access, shared living environments, or unstable internet service. These digital divides limit the reach of remote training and prevent scalable solutions from taking hold.
These roadblocks make it harder for students to train close to home, and once they leave for school, many don’t return. For hospitals, that means higher turnover, more contract labor, and a shrinking bench of homegrown talent to rely on.
A National Crisis Hiding in Plain Sight
In 2024, nearly 99 million Americans lived in federally designated Health Professional Shortage Areas (HPSAs)—regions where the supply of healthcare professionals falls short of population needs.7 While physician and nursing shortages tend to dominate the conversation, it’s the allied health workforce—which accounts for nearly 60% of all U.S. healthcare workers—that often bears the brunt of the crisis. These professionals provide essential services across diagnostics, therapy, rehabilitation, and critical care, roles that keep hospitals running and patient outcomes strong.
Yet most training programs remain concentrated in urban centers, creating enormous geographic gaps in access to education and, by extension, care. These School Deserts leave rural hospitals without a local pipeline of talent and force students to relocate or abandon healthcare careers altogether.
But geography isn't the only barrier. Even when students enroll in allied health programs, financial instability derails progress. In a recent survey, 19% of students reported dropping out, with financial uncertainty cited as the leading cause. These aren’t just individual setbacks—they represent a direct loss to our future healthcare workforce. Without targeted efforts to reduce financial strain, we risk losing tens of thousands of capable professionals before they even enter the field.8
The result: a deepening shortage that current solutions haven’t solved. According to the American Hospital Association, the U.S. is projected to face a shortfall of more than 100,000 allied health workers by 2028, and existing federal interventions have proven insufficient to meet rising demand.9
Without a major shift in how and where we develop this workforce, the consequences will ripple across every corner of the healthcare system—from emergency response and surgery to chronic care and diagnostics.
The Human Cost of School Deserts: Marc, a 75-year-old retired electrician, slipped on a patch of ice and broke his hip. After surgery and a brief hospital stay, he was medically ready for discharge to a skilled nursing facility (SNF) for rehabilitation. But like many patients, Marc found himself stuck—ready to leave the hospital, but with nowhere to go. Local SNFs were facing critical staffing shortages and had long waitlists for beds. This bottleneck—caused in part by a lack of trained allied health professionals—is increasingly common. Patients are caught in limbo, waiting for the care they need to recover, while occupying hospital beds needed for new admissions. Some states are piloting “Sub-acute at Home” programs to ease this pressure, offering remote care and in-home visits from licensed caregivers. Still, the workforce shortage has real consequences: a 2022 analysis found that patients who require skilled nursing care experience a 24% increase in hospital length of stay due to these delays. Marc’s story is not an outlier—it’s a warning. When communities lack the allied health workforce they need, patients pay the price
Role Specific Shortages At–a-Glance
The following role-specific snapshots compare projected 2030 workforce demand against the estimated supply of new graduates (2023–2030) combined with an estimate of the existing workforce, adjusted for expected annual attrition. This provides a directional view of whether states are on track to meet future clinical workforce needs of key allied health roles.
These projections offer a valuable lens into potential training pipeline gaps but do not reflect the full complexity of workforce dynamics. Notably, they exclude factors such as delayed licensure, in- or out-of-state migration, and part-time employment. As a result, actual shortages in some regions may be more severe than depicted—especially in states with aging populations, limited clinical infrastructure, or persistent out-migration of healthcare professionals.
Respiratory Therapists
The U.S. is projected to face a shortage of nearly 5,000 respiratory therapists by 2030, driven by population aging and urban-skewed education access.
- Most training programs are clustered in cities, leaving rural communities without local pathways into the field.
- Some health systems have begun deploying creative stopgaps. At Arkansas Children’s Hospital, for example, janitorial staff have been trained to take on up to one-third of respiratory therapy responsibilities as part of an upskilling initiative—an approach that reflects both innovation and desperation.
- Demand for respiratory therapists is expected to grow 13% by 2033, outpacing the average growth rate for all healthcare professions.11
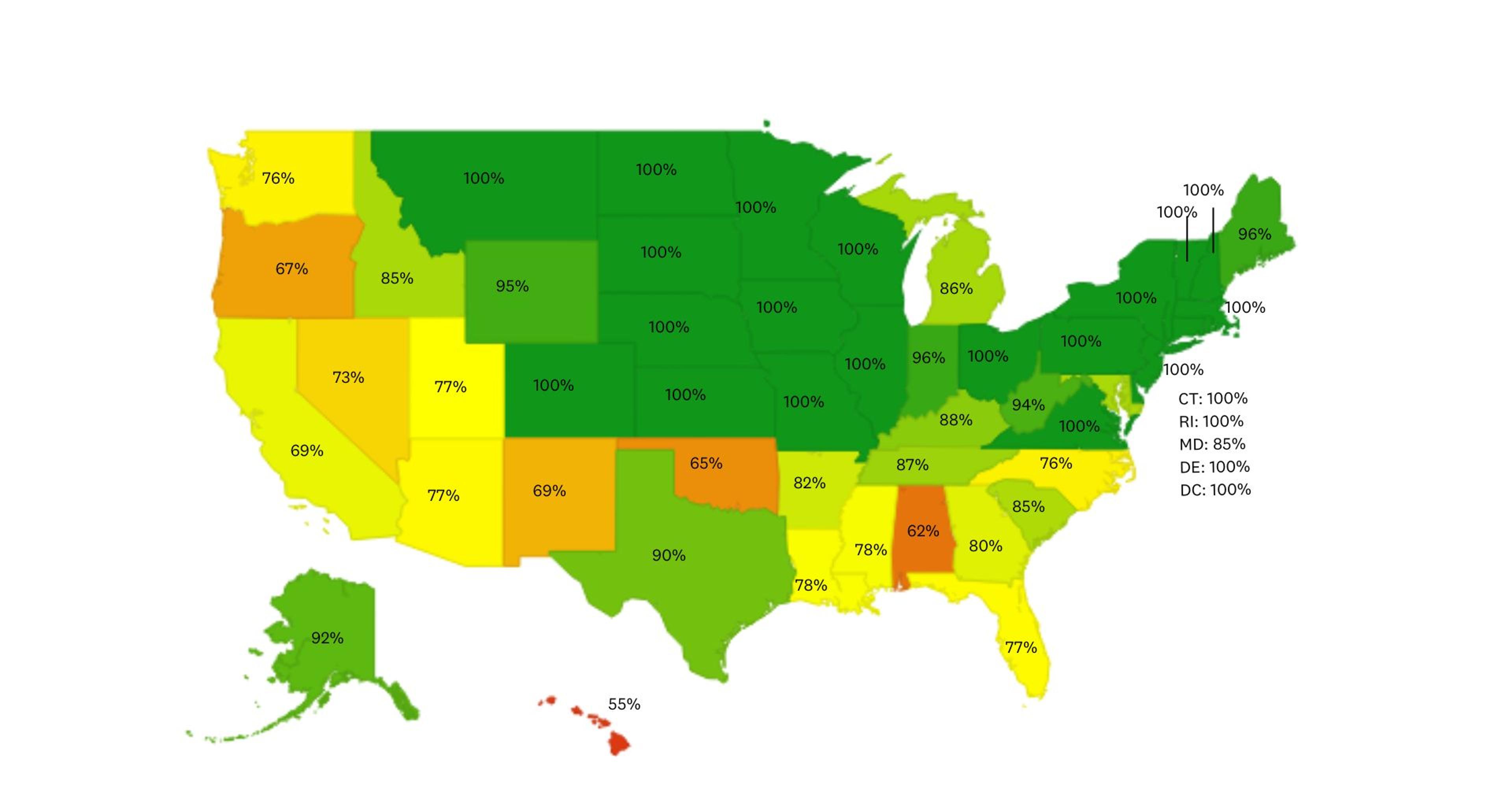
Projected 2030 Respiratory Therapist Workforce Coverage
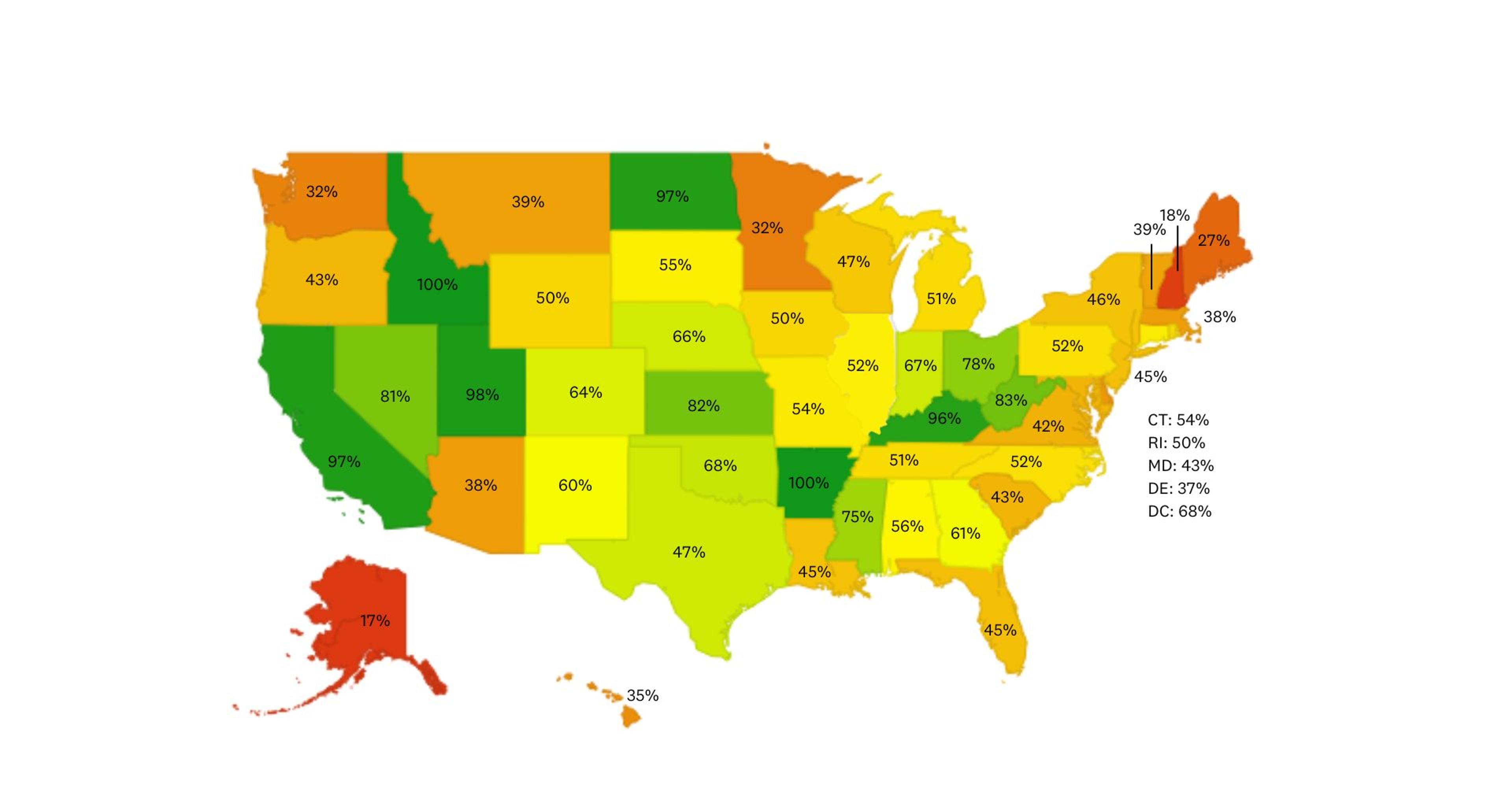
ABOUT THIS MAP: The map shows overall workforce pressure over the next five years, blending today’s supply with projected attrition and new entrants. Unlike the table, which isolates student pipeline risk, the maps capture a broader “current state” view.
Radiologic Technologists
Radiologic technologists form the essential foundation of diagnostic imaging and treatment—but many regions lack even a single accredited program. Roughly one-third of radiologic technologists complete a bachelor’s degree, while two-thirds enter the field through associate degree programs—making broad, affordable access to both pathways critical for sustaining the workforce.
Shortages extend beyond general radiography – with gaps in specialized imaging roles like MRI and CT technologists, too. These roles require additional credentialing, meaning shortages at the generalist level directly limit the ability to build a specialized workforce.
Without enough entry-level radiologic technologists, health systems will continue to struggle to fill critical, high-skill imaging positions, delaying diagnosis, increasing burnout and creating bottlenecks in patient care. Expanding access to local radiologic technology programs is not just about meeting today’s needs, it's about protecting the future imaging workforce pipeline.
- Alaska has no in-state options.12
- Most ARRT-accredited programs are concentrated in metro areas.
- The Bureau of Labor Statistics (BLS) projects a 6% growth in demand for radiologic technologists by 2031–outpacing the average growth rate for all occupations (4%)–yet access remains stagnant.13
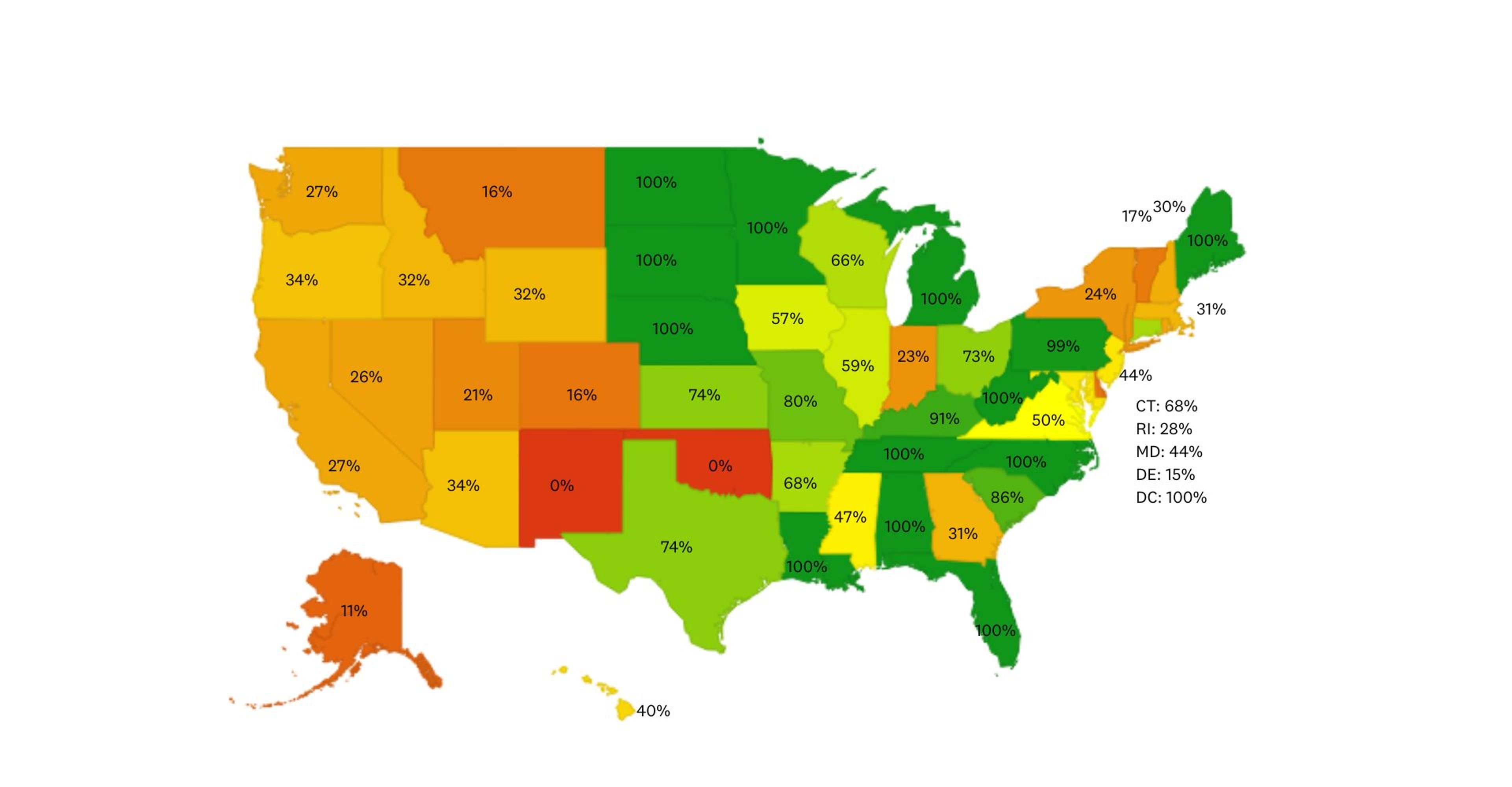
Projected 2030 Radiologic Technologist Workforce Coverage
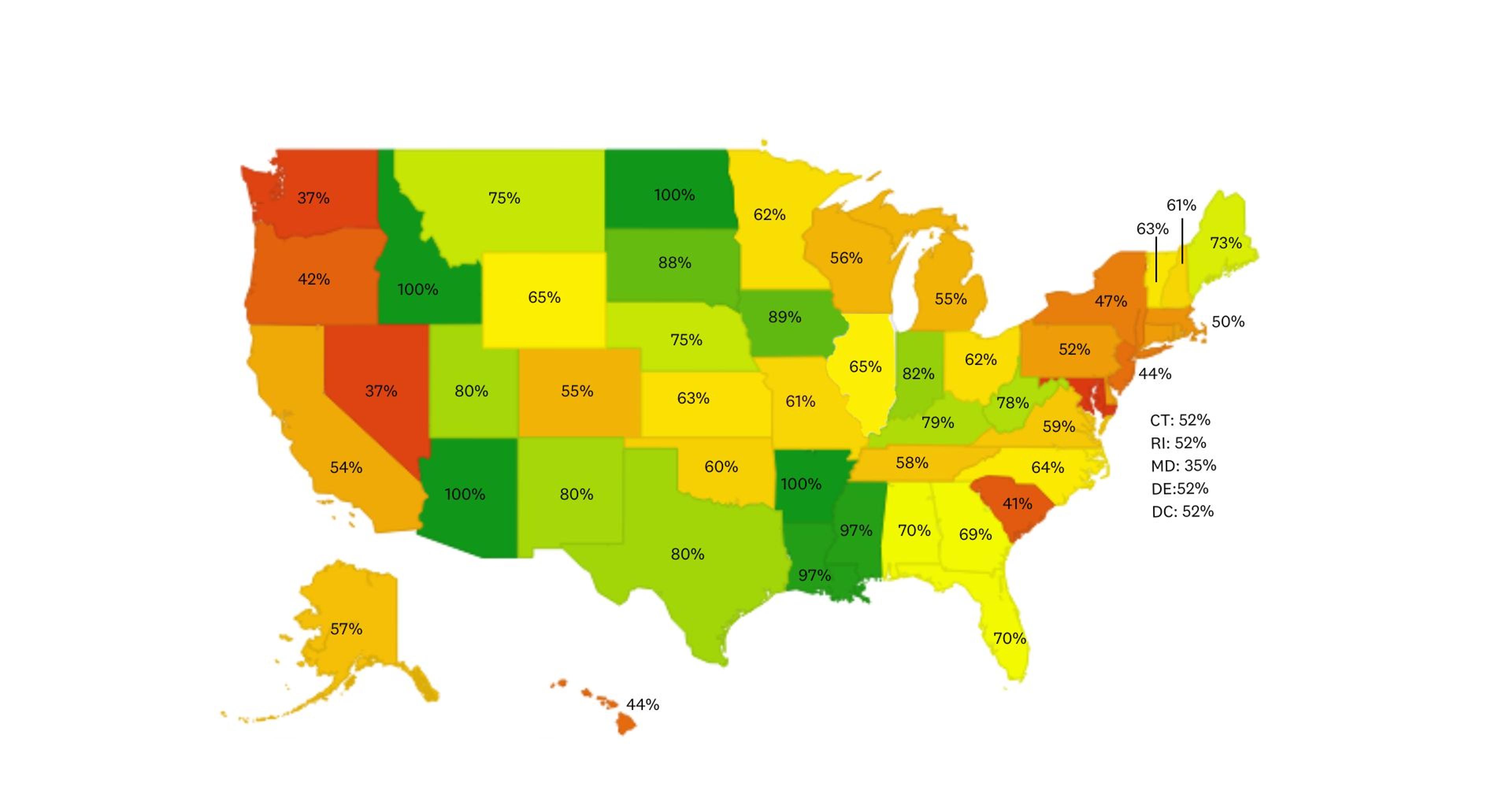
ABOUT THIS MAP: The map shows overall workforce pressure over the next five years, blending today’s supply with projected attrition and new entrants. Unlike the table, which isolates student pipeline risk, the maps capture a broader “current state” view.
Surgical Technologists
Surgical technologists are crucial to ensuring operations rooms are prepped and sterile. They keep the OR running safely, without them, surgeries simply cannot happen. In most hospitals, surgical departments are the #1 driver of revenue, making OR staff critical to both patient care and hospital financial health. But, the surgical technologist workforce is under pressure: with a growing population aging towards retirement and education enrollment dropping, 1 in 5 hospitals are already cutting OR schedules due to short staffing. Despite projected job growth of 6% by 2033—higher than the national average of 4%—access to training programs remains flat.14
Most surgical technologists enter the field through associate degree or certificate programs. But with limited access, some hospitals are stepping in—upskilling existing employees into surgical tech roles. It’s a creative way to close gaps and grow talent from within. Still, without broader support, hospitals risk canceled surgeries, lost revenue, and reduced access to critical procedures for patients.
- Roughly 40% of surgical technologists are over the age of 50, signaling a wave of upcoming retirements with too few replacements in sight.
- Enrollment in accredited surgical tech programs is down 11%, limiting the supply of new graduates just as demand is increasing. Many hospitals are increasingly relying on travelers to fill the gap.
Projected 2030 Surgical Technologist Workforce Coverage
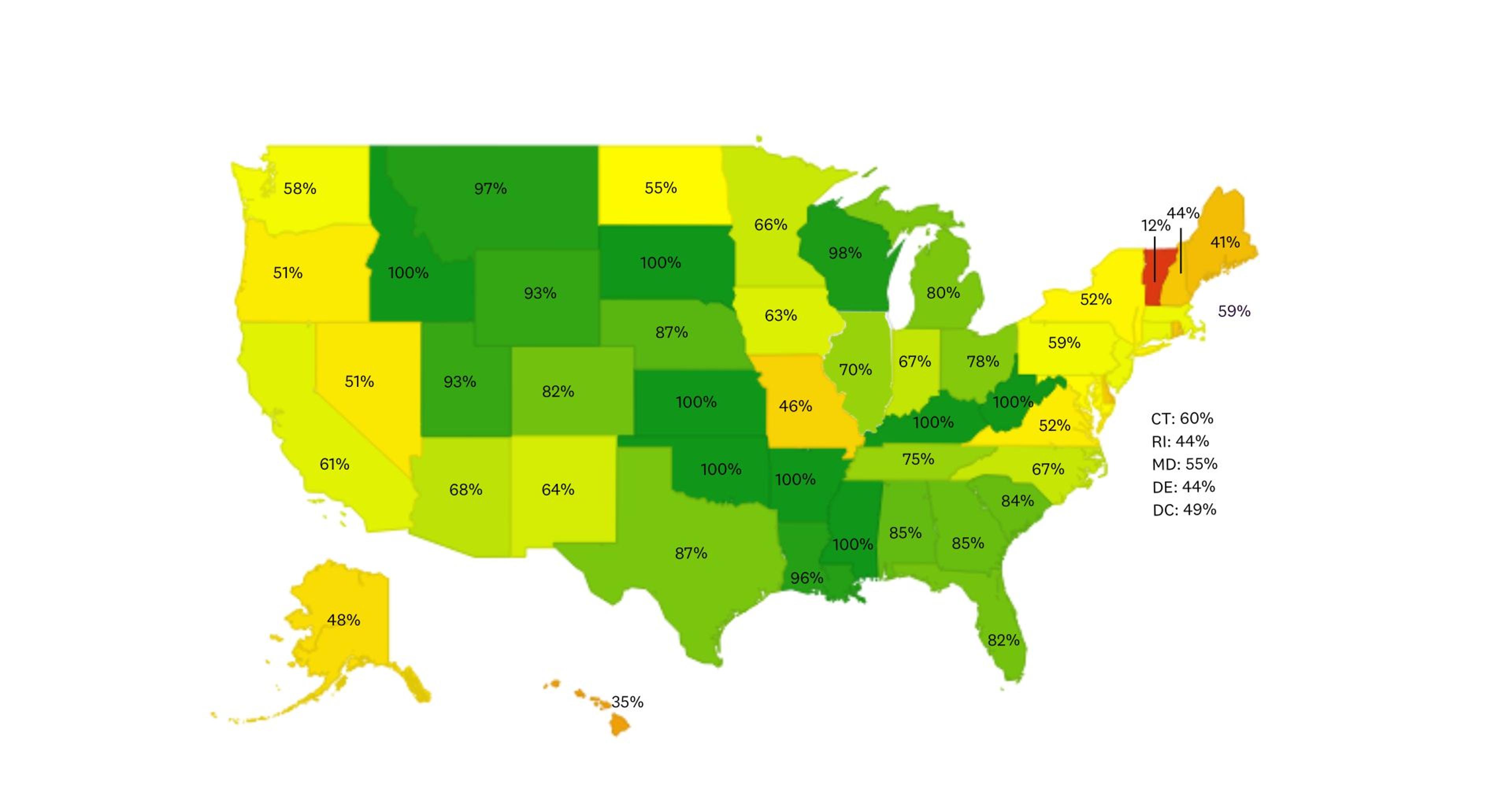
ABOUT THIS MAP: The map shows overall workforce pressure over the next five years, blending today’s supply with projected attrition and new entrants. Unlike the table, which isolates student pipeline risk, the maps capture a broader “current state” view.
Medical Laboratory Technicians
Lab techs are the backbone of diagnostic medicine, analyzing samples to help doctors reliably diagnose and treat medical conditions—but the pipeline is drastically shrinking. Many major labs are currently experiencing staff shortages and are operating in near-crisis mode.15 Rural hospitals, in particular, are facing even steeper shortages: one 2022 survey found that vacancy rates in rural hospital labs can be up to 2-3 times higher than in urban hospitals.16 When lab roles go unfilled, turnaround times for critical tests like blood work, pathology, and infectious disease diagnostics lengthen, putting patient outcomes and hospital operations at risk.
With the Bureau of Labor Statistics projecting an average 5% job growth in this field by 2032 — slightly above the national average of 4% — the gap is expected to widen if access to local training programs doesn’t improve.17
- The demand for lab techs far exceeds the number of qualified professionals. The demand continues to grow to nearly 20,000 additional roles by 2033.18
- Community colleges—key training grounds—are closing due to budget constraints.
- For rural hospitals, this means slower lab turnaround and mounting staffing gaps
Projected 2030 Lab Tech Workforce Coverage
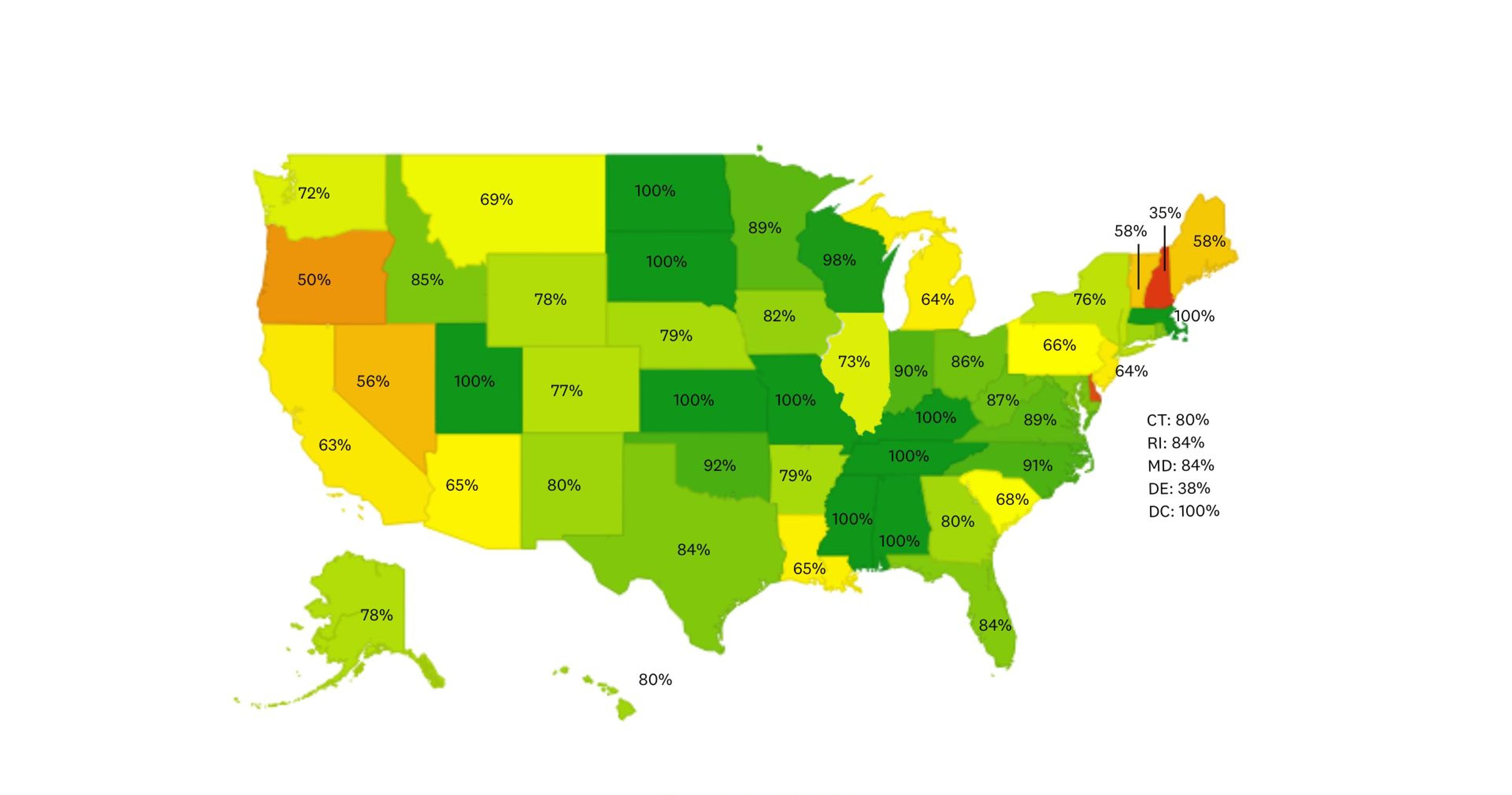
ABOUT THIS MAP: The map shows overall workforce pressure over the next five years, blending today’s supply with projected attrition and new entrants. Unlike the table, which isolates student pipeline risk, the maps capture a broader “current state” view.
Physical Therapists
Physical therapists provide critical care to patients recovering from injury, surgery, and chronic conditions. By 2030, the U.S. is projected to face a deficit of nearly 19,000 physical therapists—jeopardizing patient care and straining healthcare facilities.19
Beyond sheer numbers, the pathway to becoming a physical therapist has grown longer and more expensive. The shift to a Doctor of Physical Therapy (DPT) requirement has significantly increased the cost of education, with new graduates carrying an average debt of over $150,000, while median earnings hover around $100,000 per year.20 This means student loan payments consume a significant portion of early-career income, creating financial pressure that deters prospective students. These barriers will dissuade future students, deepening the shortage and leaving healthcare systems struggling to staff critical recovery and rehabilitation services.
- Wait times for care are increasing, particularly in underserved areas, often stretching from several weeks to multiple months.
- The aging population is driving up demand for physical therapists, not only in hospitals and outpatient clinics but also in long-term care and rehabilitation facilities, where ongoing therapy is essential to maintaining mobility and quality of life for seniors.
Projected 2030 Physical Therapist Workforce Coverage
ABOUT THIS MAP: The map shows overall workforce pressure over the next five years, blending today’s supply with projected attrition and new entrants. Unlike the table, which isolates student pipeline risk, the maps capture a broader “current state” view.
Nurse Anesthetists
Nurse Anesthetists (CRNAs) play a pivotal in delivering anesthesia care, especially in rural and underserved areas where they often serve as the primary or sole providers. Their advanced training enables them to administer safe, high-quality, and cost-effective anesthesia services, ensuring that surgical and obstetric procedures remain accessible in these communities.
However, the pathway to becoming a CRNA has become more challenging, with a requirement for a doctoral degree increasing both the cost and length of education. This raises barriers for prospective students and limits the growth of the workforce.
- The current shortage of CRNAs is severe—projected to be more than four times the number of all expected graduates in 2025 (about 12,500), intensifying staffing challenges nationwide.
- Many CRNA training programs are clustered in urban areas, creating geographic imbalances that limit access for rural students.
- States like Alaska and Montana lack in-state CRNA programs. This absence of local training programs exacerbates provider shortages in these regions.21
Projected 2030 Nurse Anesthetist Workforce Coverage
ABOUT THIS MAP: The map shows overall workforce pressure over the next five years, blending today’s supply with projected attrition and new entrants. Unlike the table, which isolates student pipeline risk, the maps capture a broader “current state” view.
State Spotlights: Where School Deserts Hurt Most
New Mexico: Distance Deepen the Divide
Geography and underserved populations make New Mexico’s healthcare workforce especially vulnerable. A recent report from Think New Mexico estimates a 52% workforce shortfall by 2035—a deficit of 3,400+ allied health workers.22
Key challenges include:
- Long commutes—3+ hours from counties like Catron and Union to Albuquerque or Las Cruces
- No accredited programs in many rural and Native-serving areas
- Minimal clinical capacity for lab-heavy fields
- High dropout rates due to distance and infrastructure challenges
Proposed solutions include simulation-based learning and tribal partnerships, but implementation has been slow.
Colorado: A Corridor of Concentration
While Colorado produces a significant number of allied health graduates, nearly all programs are clustered along the Front Range—Denver, Boulder, and Colorado Springs.23 This leaves vast regions like the San Luis Valley and Eastern Plains with:
- 2–3 hour commutes to reach the nearest training program
- A lack of clinical placement capacity in rural hospitals
- Rising vacancies and dependence on traveling staff
Without regional training infrastructure, the rural workforce pipeline remains fractured.
Florida: A State of Contrasts
Florida's rapidly growing and aging population is intensifying the demand for allied health professionals. Urban hubs like Tampa, Orlando, and Miami are well-served—but rural counties fall far behind. This mismatch is worsening provider shortages across the state.
- The urban-rural gap isn't just geographic— it's structural. Clinical placements, faculty shortages, and strained provider partnerships make it harder for programs outside metro areas to scale.
- High turnover rates among allied health professionals in Florida are fueling workforce shortages: With roles like surgical technologists and medical assistants experiencing turnover as high as 22-24%, frequent staff churn disrupts care delivery and deepens gaps in an already strained system.24
The Florida State Office of Rural Health has flagged this urban-rural divide as a top concern.25
Mississippi: Shrinking Supply, Despite Investment
Mississippi has one of the lowest densities of allied health program in the country, leading to severe shortages in:
- Respiratory therapists
- Physical therapy
- Nurse Anesthetist
Many students leave the state for training—and don’t return. A $15M investment in 2022 expanded allied health and nursing programs at HBCUs and community colleges.26 Still significant challenges remain:
- Rural regions face long recruitment cycles and persistent staffing gaps, driving up costs and straining the delivery of care.
- Clinical placement opportunities remain limited, even as the state expands allied health education programs—hindering efforts to train and retain a local workforce.
Sustainable progress will require more local infrastructure—not just funding.
Georgia: A Tale of Two Cities
Metro Atlanta is rich in training options, but 46 of Georgia’s 159 counties lack even a single allied health program.27 This gap fuels severe shortages in the southwest and northeast, where:
- The current student pipeline is not large enough to fill new positions
- Some students travel 100+ miles for clinical training
- Broadband and outdated school facilities limit hybrid learning potential
The state is piloting loan repayment and apprenticeship models—but barriers to access remain high outside of urban centers.
Want to dive deeper into your state’s allied health workforce landscape? We offer custom briefings across all 50 states—including localized data, role-specific shortages, and school outreach strategies. Contact us at marketing@clasp.com to request a tailored analysis or explore how Clasp can help build your regional talent pipeline.
Why Allied Health Professionals Relocate
Allied health workers move for many reasons. Understanding what drives relocation can help shape smarter workforce strategies, especially in rural areas.
- Scope of Practice: State laws vary widely in what professionals are allowed to do. For example, physical therapists relocate based on whether states allow direct patient access without a referral.
- Compensation & Incentives: Pay matters, but so do perks. Programs like the National Health Service Corps (NHSC) and Missouri’s loan repayment initiatives offer up to $50,000 to professionals working in high-need areas.28
- Work-Life Balance: Professionals are more likely to stay where they feel supported. Rural programs that prioritize team-based care, mentorship, and manageable patient loads—like those in Arkansas and Iowa—have seen better retention.
- Cost of Living: A higher salary doesn’t always mean better quality of life. California pays well, but housing costs are steep. States like Texas and Tennessee offer a better balance—affordable living with solid wages.
- Professional Growth: Ongoing learning and networking matter. States with strong professional associations and training events—like Pennsylvania—attract those looking to advance their careers.
- Licensing & Mobility: Agreements between states that streamline the licensing process for professionals make it easier to move and practice. Physical therapists benefit from this across 34 states. But for others, like radiologic technologists, extra licensing hurdles can be a barrier.
Recognizing these factors helps guide smarter recruitment, policy, and support systems—especially in communities that need healthcare talent the most.
The Financial Toll on Health Systems
When allied health training programs disappear from a region, the impact on healthcare employers goes far beyond staffing headaches—it directly affects the bottom line. These “school deserts” increase costs and create operational strain in already resource-limited settings. Every unfilled clinical role creates significant costs for health systems, including lost revenue, increased overtime expenses, and heavy reliance on costly contract labor—putting financial strain on both operations and patient care. Without a local pipeline of trained professionals, hospitals are left competing for a shrinking talent pool—at a premium. These systems face:
- Rising vacancy costs. Unfilled roles mean higher overtime, lost productivity, and delays in care.
- Heavier reliance on contract labor. Travel staff may plug holes, but at 2–3x the cost of permanent hires, they strain budgets and often lack long-term commitment.
- Reduced service capacity. Persistent shortages force some hospitals to close beds or delay procedures, directly impacting patient care and revenue.
- Underutilized local talent. Without nearby training options, many potential candidates leave the region—or never enter the field to begin with.
What Systems Can Do Now: 4 High-Impact Strategies
Tackling allied health shortages in underserved regions requires more than short-term recruitment tactics. The most effective health systems are shifting from reactive hiring to proactive workforce development. Here's how:
1. Grow Talent Through Local Training Hubs
Make it possible for students to train—and stay—local.
What to do:
- Partner with community colleges or universities to create rural satellite programs. Institutions like Drexel University, Manchester Community College and Baylor University are already doing this!
- Use existing hospital space for classrooms, labs, or simulation centers.
- Prioritize training programs that align with the highest local demand and workforce shortages.
Why it works:
Students trained in their own communities are significantly more likely to stay and serve locally, reducing turnover and staffing gaps.
2. Build Hybrid Learning Infrastructure
Reduce the travel burden and bring training closer to home.
What to do:
- Invest in broadband, simulation labs, and preceptors onsite at hospitals
- Partner with online or hybrid training providers to combine virtual coursework with in-person clinical experiences
- Explore innovative simulation tools, like Chamberlain's AI-powered platforms like SIMCARE, which offer immersive, hands-on experiences that complement remote learning.
Why it works: Hybrid learning helps students complete coursework remotely while gaining clinical experience locally—lowering dropout risk and strengthening the pipeline.
3. Incentivize Rural Learners
Remove the cost barriers that prevent students from entering the field.
What to do:
- Offer student loan repayment via Clasp in exchange for post-grad commitments
- Provide housing or travel stipends during training
- Pilot paid clinical internships or scholarships for high-need specialties
Why it works: Financial stress keeps many qualified students out of allied health fields. Strategic incentives help retain talent and ensure ROI on workforce investments.
4. Train the Trainers: Expand Educator Capacity
Without faculty, programs can’t grow—no matter the demand.
What to do:
- Support clinical staff who want to teach with mentorship and tuition reimbursement
- Build “train-the-trainer” programs in regions
- Dedicate time and funding for part-time instruction roles
Why it works: Programs often hit bottlenecks due to instructor shortages. Investing in educator pipelines enables sustainable program expansion over time.
Want help putting these strategies into action? Clasp partners with health systems to launch sustainable education-to-career programs in underserved communities. Reach out to marketing@clasp.com to learn more.
The Bottom Line
School deserts aren’t just an education problem—they’re a workforce crisis. Hospitals in affected regions face prolonged vacancies, higher recruiting costs, and reduced care access. But there’s a path forward.
Health systems that act now—by investing in training infrastructure, hybrid access, and retention-based incentives—can build a future-ready pipeline. The ROI is clear: fewer vacancies, stronger teams, and deeper local ties.
At Clasp, we partner with healthcare systems and schools to launch education-to-career pathways that reduce barriers, attract emerging talent, and incentivize 3+ years of retention. By analyzing migration patterns, we help widen clinical candidate pools—recently enabling a partner to attract CRNA applicants from 14 states within less than one quarter, demonstrating how expanding beyond local markets can quickly address critical workforce shortages.
Let’s fix the pipeline—together.Contact us to explore how Clasp can support your allied health hiring and retention strategy. Set up a meeting today.



About Clasp
for Healthcare Employers
Clasp is on a mission to tackle the healthcare talent shortage. We help healthcare organizations, systems, and hospitals across the country reach talent earlier, keep them longer, and invest in them smarter — drastically reducing turnover and the traditional costs of recruiting.
How? Through innovative recruiting programs that leverage student loan repayment and in-school employment commitments to attract and retain talent before they even graduate.
Learn More
References
1. National Rural Health Association(NRHA). Workforce Series: Allied Health. https://www.ruralhealth.us/getmedia/ff186532-f395-4a93-a69c-7718aae34e7f/WorkforceAlliedHealth.pdf
2. American Association of Nurse Anesthesiology. What is the CRNA/nurse anesthesiologist job outlook? https://www.aana.com/motion-crna-career-platform/what-is-the-crna-nurse-anesthesiologist-job-outlook/
3. WWMT News. Radiologist shortage forces Michigan patients to wait months for medical test results. https://wwmt.com/news/i-team/radiologist-shortage-investigative-journalism-health-issues-community-kalamazoo-county-west-michigan
4. University of New Hampshire. Growing Racial Diversity in Rural America: Results from the 2020 Census. https://carsey.unh.edu/publication/growing-racial-diversity-rural-america-results-2020-census
5. HRSA Health Workforce. State of the U.S. Health Care Workforce, 2024. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/state-of-the-health-workforce-report-2024.pdf
6. Post Crescent. Spectrum continues to expand high-speed internet to rural communities west of Appleton. https://www.postcrescent.com/story/money/companies/2025/02/28/outagamie-winnebago-county-communities-see-spectrum-expansion/80837470007/
7. Health Resources and Services Administration (HRSA). Workforce Projections. https://data.hrsa.gov/topics/health-workforce/workforce-projections
8. Ellucian. National Survey Reveals 59% of College Students Consider Dropping Out Due to Financial Stress. https://www.ellucian.com/news/national-survey-reveals-59-college-students-considered-dropping-out-due-financial-stress
9. American Hospital Association. 5 Health Care Workforce Shortage Takeaways for 2028. https://www.aha.org/aha-center-health-innovation-market-scan/2024-09-10-5-health-care-workforce-shortage-takeaways-2028
10. KFF Health News. Sent Home To Heal, Patients Avoid Wait for Rehab Home Beds. https://kffhealthnews.org/news/article/patients-rehab-at-home-unclog-hospital-bed-nursing-home-waiting-list/
11. Bureau of Labor Statistics. Occupational Outlook Handbook - Respiratory Therapists. https://www.bls.gov/ooh/healthcare/respiratory-therapists.htm#tab-6
12. Joint Review Committee on Education in Radiologic Technology. Radiologic Technologists Schools. https://www.jrcert.org/wp-content/uploads/articulate_uploads/Organizational-Reports-2-20-25/JRCERT%20Organizational%20Reports.html#p=23
13. Bureau of Labor Statistics (BLS). Occupational Outlook Handbook. Radiologic and MRI Technologists. https://www.bls.gov/ooh/healthcare/radiologic-technologists.htm
14 .Bureau of Labor Statistics (BLS). Occupational Outlook Handbook. Surgical Assistants & Technologists.
15. American Society for Clinical Pathology and ASCP Board of Certification. Hearing on “Examining Health Care Workforce Shortages: Where Do We Go from Here?” https://ascpcdn.s3.amazonaws.com/static/epolicy/2023/ASCP+%26+ASCP+BOC+Statement+on+Senate+HELP+Committee+Hearing+on+Examining+Health+Care
16. National Library of Medicine. The American Society for Clinical Pathology 2022 Vacancy Survey of medical laboratories in the United States. https://pubmed.ncbi.nlm.nih.gov/37936416/#:~:text=Results%3A%20Results%20of%20the%20ASCP,professionals%20increased%20across%20most%20departments
17. Bureau of Labor Statistics. Clinical Laboratory Technologists and Technicians. https://www.bls.gov/ooh/healthcare/clinical-laboratory-technologists-and-technicians.htm
18. US News. Clinical Laboratory Technician Overview. https://money.usnews.com/careers/best-jobs/clinical-laboratory-technician#:~:text=The%20Bureau%20of%20Labor%20Statistics,18%2C200%20jobs%20should%20open%20up
19. American Physical Therapy Association. PTJ: New Workforce Forecast Projects PT Shortages Through 2037. https://www.apta.org/news/2025/03/04/workforce-forecast-2022-2037#:~:text=There%20was%20a%20national%20shortfall,term%20care%20(8.9%25)%20settings
20. American Physical Therapy Association. Impact of Student Debt on the Physical Therapy Profession. https://www.apta.org/contentassets/ee2d1bb7f9d841c983d0f21bb076bb79/impact-of-student-debt-report.pdf
21. All CRNA Schools. CRNA Schools by State. https://www.all-crna-schools.com/nurse-anesthesia-crna-schools-by-state/#states-1
22. Think New Mexico. Healthcare Workforce Shortage. https://www.thinknewmexico.org/health-care-worker-shortage/
23. SLVAHEC. Providing important services to underserved populations. https://www.slvahec.org
24. Florida Hospital Association. New Data Reveals Significant Improvemetns to Florida's Health Care Workforce Shortage. https://www.fha.org/FHA/FHA/News-Content/New-Releases/091224%20Vacancy%20and%20Turnover%20Data%20Release.aspx
25. Florida State Office of Rural Health. Rural Health Needs Assessment. https://www.floridahealth.gov/programs-and-services/community-health/rural-health/index.html
26. Accelerate Mississippi. Accelerate Mississippi Nursing/ Allied Health Grant Program. https://impact.acceleratems.org
27. Georgia Healthcare Workforce Commission. Georgia Healthcare Workforce Commission Executive Summary.
28. Health Resources and Services Administration (HRSA). Loan Repayment Programs for Health. https://bhw.hrsa.gov/funding/apply-loan-repayment
29. Medix. What Your Open Healthcare Positions Are Costing Your Organization. https://www.medixteam.com/blog/what-your-open-healthcare-positions-are-costing-your-organization/
Data Sources
Physical Therapist Graduates (2024): https://www.capteonline.org/globalassets/capte-docs/aggregate-data/2024-pt-aggregate-program-data-fact-sheet.pdf
Radiologic Technologists Schools: https://www.jrcert.org/wp-content/uploads/articulate_uploads/Organizational-Reports-2-20-25/JRCERT%20Organizational%20Reports.html#p=23
Respiratory Therapist Schools: https://coarc.com/students/find-an-accredited-program/
Estimated workforce projections by role: https://data.hrsa.gov/topics/health-workforce/workforce-projections
2023 Graduation Data by role: https://nces.ed.gov/ipeds/datacenter/CDSPreview.aspx?sid=efeb6eb2-d3c8-470e-852e-06e5ce15535d&rtid=5
Nurse Anesthetist attrition rate: https://dhhs.ne.gov/licensure/Credentialing%20Review%20Docs/CRAASurveyArticle-AANAJournalDec2021.pdf
Respiratory Therapist attrition rate: https://respiratory-therapy.com/public-health/healthcare-policy/respiratory-therapist-shortage-invest-in-rts-today/#:~:text=RT%20turnover%20is%20sharply%20increasing,up%20from%2012%25%20in%202019
Radiologic Technologist attrition rate: https://www.linkedin.com/pulse/reducing-employee-turnover-radiology-eason-dba-rt-r-cra/
Physical Therapist attrition rate: https://www.apta.org/contentassets/787bafc2ef664074ace8914f748ee4cd/apta-2025-workforce-forecast-companion-report.pdf