Nursing "Not a Professional Degree"? What's Actually Changing — And How Hospitals Can Respond
WEBINAR REPLAY | 12.12.2025
Federal graduate loan caps are changing. Here’s what that actually means for healthcare employers.
Over the past few weeks, headlines about federal student loan changes have sparked confusion, anxiety, and more than a few misleading takes — especially across healthcare.
Terms like “nursing is no longer a professional degree” grabbed attention, but missed the real story.
What’s actually changing isn’t the value of healthcare roles. It’s how much students will be allowed to borrow from the federal government to access them — and that shift has serious implications for the future clinical workforce.
What’s changing (in plain English)
Beginning in 2026, proposed federal rules would place new limits on how much graduate students can borrow through federal loans.
Under these changes:
- Most graduate students would be capped at ~$100,000 in total lifetime borrowing
- Annual borrowing limits would also apply
- Many healthcare degrees — including several APP and allied-health roles — would not qualify for higher “professional degree” limits
On paper, this looks like a reasonable attempt to rein in rising education costs.
In practice, it collides with the reality of healthcare training.
Why healthcare is uniquely exposed
Healthcare education isn’t optional or flexible.
Licensure requires:
- Multi-year programs
- Mandatory clinical hours
- Limited program capacity
- Strict accreditation standards
At the same time, tuition has continued to rise — especially at private and capacity-constrained programs.
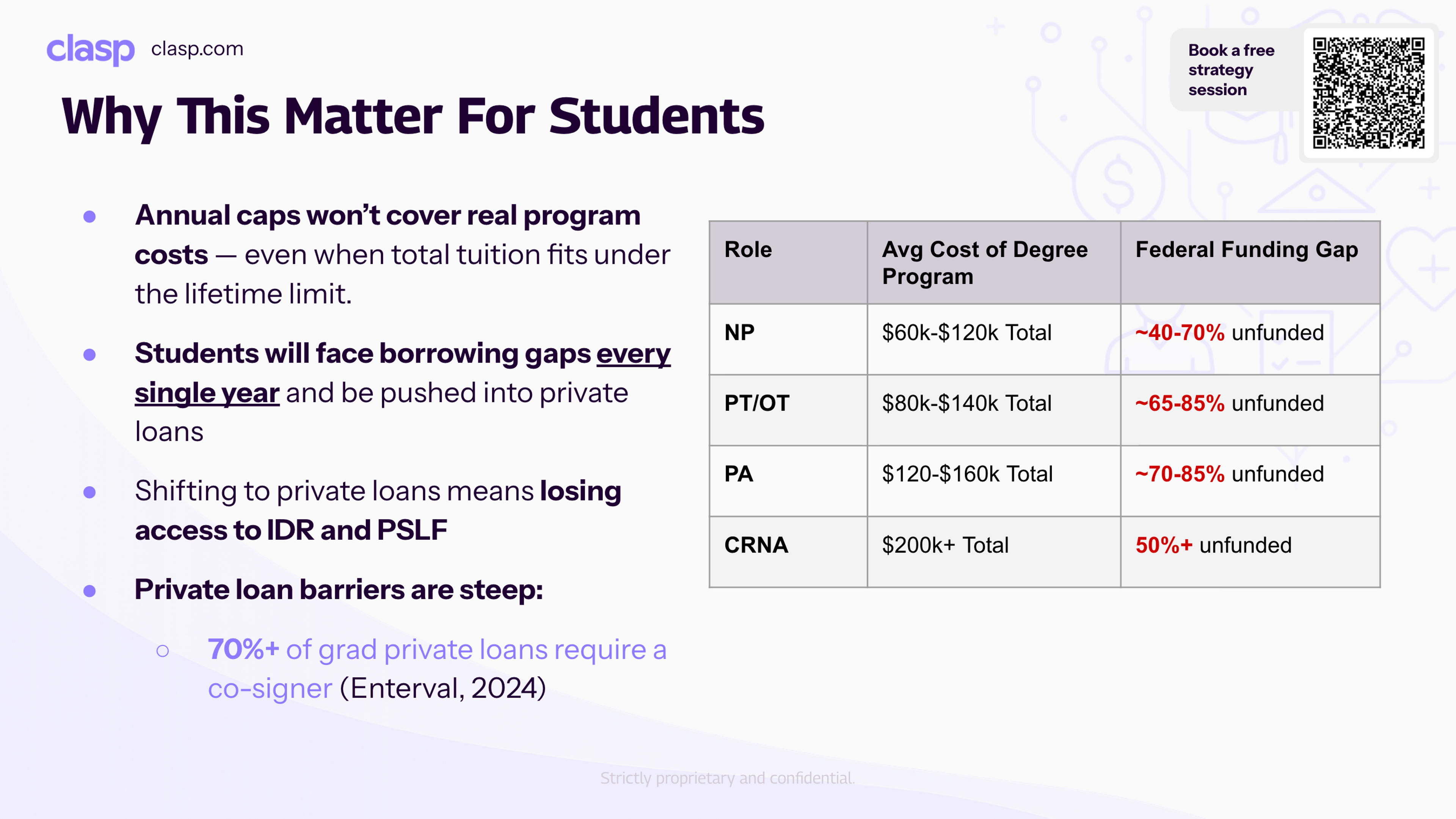
Today, many APP and allied-health graduate degrees routinely cost $140,000–$200,000 or more.
Under proposed federal caps, that means 40–85% of training could go unfunded.
This isn’t a budgeting inconvenience. It’s a financing gap large enough to stop students from enrolling at all.
What happens when federal loans run out
When students hit federal borrowing limits, their options narrow quickly:
They can attempt to secure private loans — which:
- Require cosigners in ~70% of graduate cases
- Are often inaccessible to first-gen or lower-income students
- Remove access to IDR and PSLF protections
Or they delay, downshift, or abandon clinical training entirely.
The result isn’t just fewer students. It’s a different mix of who can afford to enter healthcare.
Why this matters to employers
For healthcare employers, this shift shows up in three ways:
First, pipelines shrink. Fewer students can afford to enroll, and fewer graduates reach the market.
Second, shortages get more expensive. When supply tightens, recruiting costs rise — and competition intensifies.
Third, access and diversity take a hit. When financing depends on family wealth or cosigners, entire populations are quietly pushed out of clinical careers.
By the time this shows up as vacancy pain, it’s already too late to fix reactively.
What proactive employers are doing differently
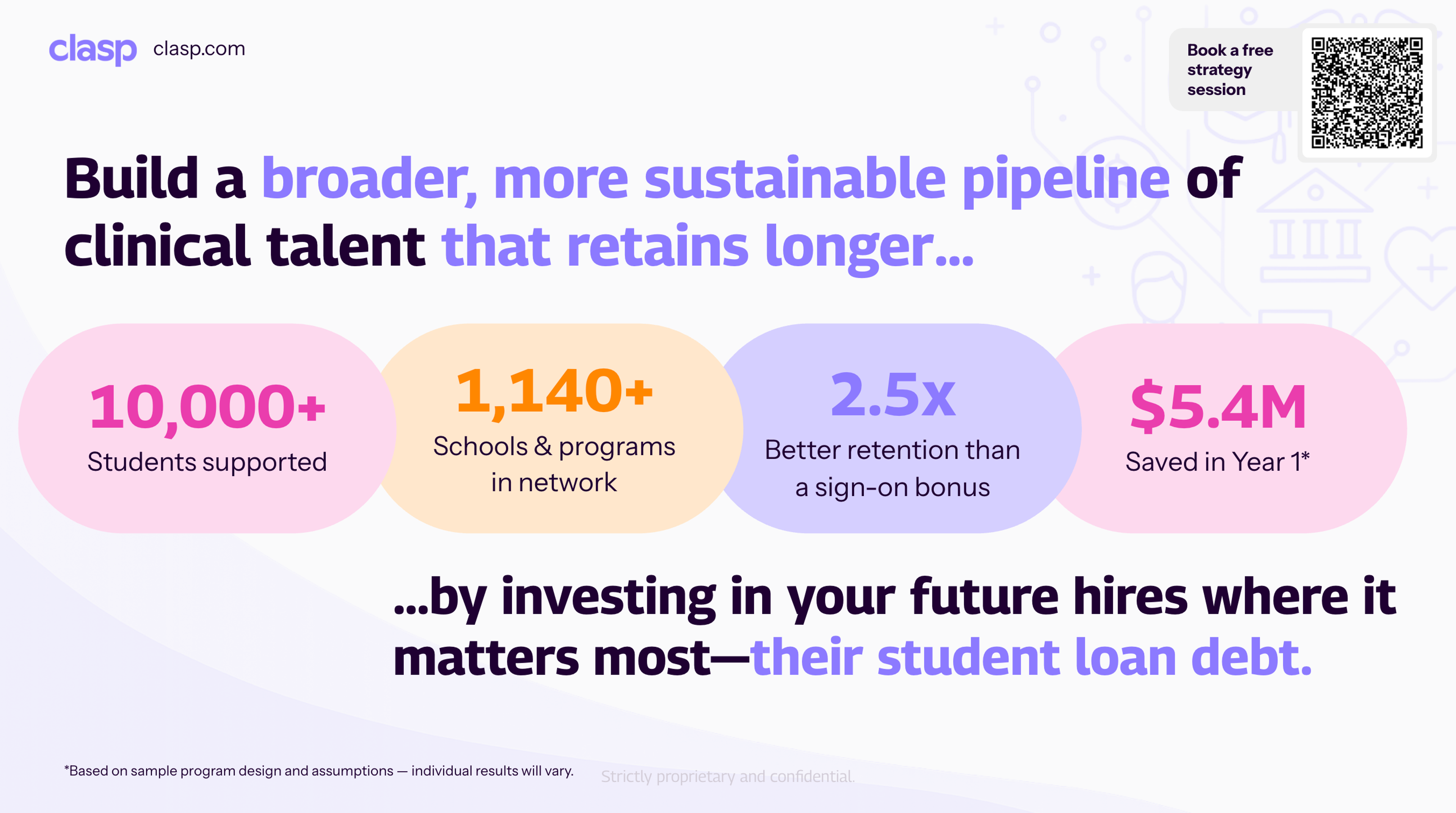
Some healthcare systems aren’t waiting for 2026 to act. They’re:
- Engaging talent earlier, while students are still in training
- Offering post-hire student loan repayment instead of upfront tuition
- Using loan support to drive multi-year retention, not just signing
- Partnering with schools to stabilize enrollment and outcomes
Rather than asking students to take on more risk, these employers are sharing it — and protecting their future workforce in the process.
And they’re doing it through Clasp, using employer-sponsored student loan repayment to secure pipelines earlier, improve access, and retain clinicians longer.
Why timing matters now
Even though federal caps wouldn’t take effect until 2026, decisions are already happening.
Students applying today are running the numbers.
Schools are watching yield risk rise.
Employers who move early gain access to talent others won’t.
This is a slow policy change with fast workforce consequences.
Watch the full conversation
In a recent Clasp webinar, Tess Michaels (CEO, Clasp) was joined by Matt Tower (VP, Strategy & Research, Whiteboard Advisors) and Stephen Clark (Chief Clinical Officer, Confluent Health) to unpack:
- What’s actually changing under proposed federal graduate loan caps
- Which healthcare roles are most exposed
- How employers are responding now — before talent pipelines tighten further
🎥 Watch the full webinar here.
Want to understand what this means for your workforce?
Every health system’s exposure looks different — depending on role mix, hiring geographies, and where your pipelines come from.
If you’re thinking about:
- How federal loan caps could impact your future hiring
- Whether employer-sponsored loan repayment makes sense for your roles
- How to protect pipelines before shortages worsen
👉 Book a free strategy session with Clasp to walk through your workforce goals, risk areas, and options — no pressure, just clarity.
Book a Free Strategy Session